CGM and Medicaid: Who’s Covered?
Continuous glucose monitoring coverage varies widely by state Medicaid program – check out our guide on who’s covered and where.
California is the most recent state to expand access to continuous glucose monitors (CGMs) under their Medicaid program, Medi-Cal. While Medi-Cal originally limited CGM coverage to children with diabetes, it has expanded CGM coverage to cover all people with type 1 diabetes. The policy will go into effect in January 2022 In California, 25% of the population is covered under Medi-Cal and the Children’s Health Insurance Program (CHIP), which are programs for low-income Americans supported by federal and state governments. We estimate that at least half of these beneficiaries have diabetes, prediabetes, or undiagnosed diabetes. For these individuals, coverage of diabetes drugs and technology dramatically increases their chances of living a life free of complications.
Despite these advancements in CGM access under Medi-Cal, California and 22 other states still do not cover CGMs for all people with diabetes who need them. CGMs are vital in providing regular blood glucose readings to track time spent in range, identifying patterns in behaviors and blood glucose, and anticipating hypo and hyperglycemia. These devices nearly eliminate the need for finger sticks and have been shown to be superior to self-monitoring of blood glucose in lowering A1C, reducing hypoglycemia, and increasing time in range in both people with type 1 diabetes and people with type 2 diabetes using insulin. In turn, these improved glycemic outcomes and increased time-in-range lead to fewer hospitalizations and long-term complications, generating substantial savings for the healthcare system.
CGMs are covered by most private insurance and also under Part B of Medicare, a federal health insurance program that covers those who are 65 or older, or who are disabled. It seems clear that the CGM benefits summarized above should be made available to everyone on Medicaid, and many in the advocacy community are working to ensure progress is made on this front.
Who is covered by Medicaid?
While Medicare benefits are the same throughout the country, Medicaid, which covers mainly low-income adults, children, pregnant women, and some parents, varies from state to state. In states that have chosen to expand Medicaid under the Affordable Care Act (ACA), people can qualify for Medicaid if their income level is below 133% of the federal poverty level. Therefore, in states that have expanded Medicaid, more people are covered and insured. In states without expansion, many people neither qualify for Medicaid nor are able to afford a subsidized private health plan through the Health Insurance Marketplace.
To find out if you qualify for Medicaid in your state, click here.
Does my state’s Medicaid program cover CGM?
It depends. In states that have expanded Medicaid, more people with diabetes are able to access Medicaid coverage benefits, which may include CGM access depending on the state. But even if CGM is covered under your state’s policy, each state has its own criteria for which individuals qualify to receive it. For example, some states only cover CGM for type 1 diabetes, and other states have differing policies for short-term and long-term CGM use. To find out more about your specific state’s policy, see the map below:
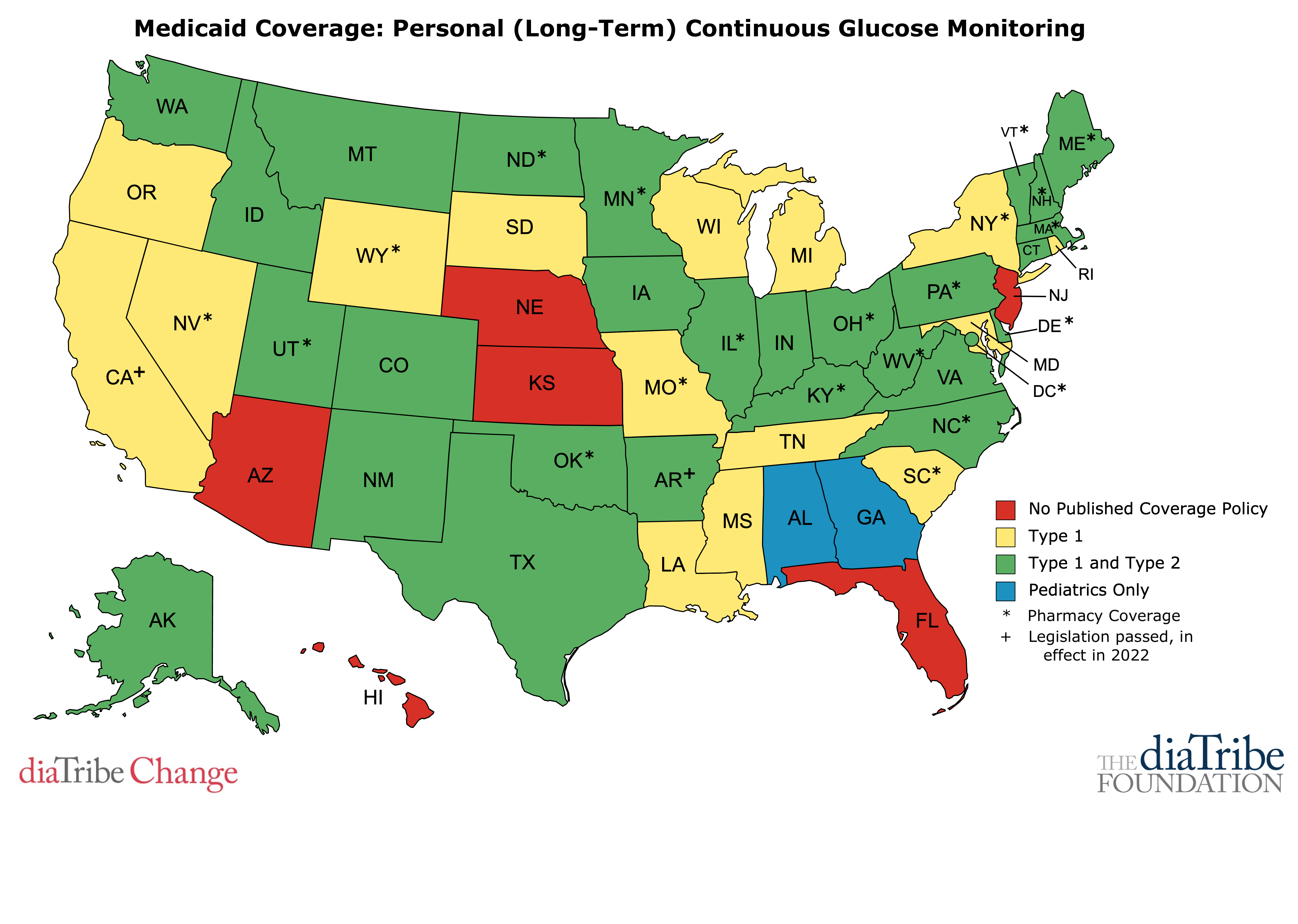
This map is the general landscape of Medicaid coverage for CGM. The 6 states shown in red (Arizona, Florida, Hawaii, Kansas, Nebraska, and New Jersey) offer no published coverage policy of CGM for Medicaid recipients, while the other states offer some degree of coverage, as shown in the legend.
15 states’ Medicaid programs provide CGM for people with type 1 diabetes only: California (in effect in 2022), Louisiana, Maryland, Michigan, Mississippi, Missouri, Nevada, New York, Oregon, Rhode Island, South Carolina, South Dakota, Tennessee, Wisconsin, and Wyoming.
27 states’ Medicaid programs (and DC) provide CGM for people with both type 1 and type 2 diabetes: Alaska, Arkansas (in effect in 2022), Colorado, Connecticut, Delaware, Idaho, Illinois, Iowa, Indiana, Kentucky, Maine, Massachusetts, Minnesota, Montana, New Hampshire, New Mexico, North Carolina, North Dakota, Ohio, Oklahoma, Pennsylvania, Texas, Utah, Vermont, Virginia, Washington, and West Virginia.
2 states’ Medicaid programs provide CGM for children only: Alabama and Georgia.
While 44 states have some coverage for CGM, a series of eligibility criteria limit access to these devices. Almost all states require at least a diagnosis of diabetes, regular visits with an endocrinologist or other healthcare provider, and self-monitoring of blood glucose at least three times per day. Many states have more limiting eligibility criteria. Even for the green states above, many people on Medicaid do not have access to a CGM because they do not meet state eligibility requirements. Here are a few examples of these criteria:
- An A1C higher than 7 or 8 percent
- Frequent experiences with severe low blood sugar
- Multiple daily injections of insulin
- CGM prescribed by an endocrinologist
Every requirement described above acts as a barrier to CGM for people with diabetes. This map provides an overview of Medicaid CGM coverage in the US but keep in mind that coverage varies by state and many factors contribute to your eligibility for a CGM. To get a definitive answer about whether you are covered, please consult your healthcare provider or your insurance plan benefits document.
Which states have the best, most inclusive Medicaid coverage of CGM?
State policies that cover CGM through a pharmacy benefit, as opposed to a medical benefit, generally make it easier for people to obtain CGM. Currently, 20 states and DC provide CGM through a pharmacy benefit: Delaware, Illinois, Kentucky, Maine, Massachusetts, Minnesota, Missouri, Nevada, New Hampshire, New York, North Carolina, North Dakota, Ohio, Oklahoma, Pennsylvania, South Carolina, Utah, Vermont, West Virginia, and Wyoming.
Of these states, Delaware, Illinois, Kentucky, Maine, Massachusetts, Minnesota, New Hampshire, North Carolina, North Dakota, Ohio, Oklahoma, Pennsylvania, Utah, Vermont, West Virginia, and DC cover CGM for people with both type 1 and type 2 diabetes, making their policies the most effective and far-reaching of the fifty states.
Getting a CGM through a pharmacy benefit is typically faster, more convenient, and less expensive for the patient. While both pharmacy and medical benefits require a doctor’s prescription, medical benefits usually require a great deal more paperwork and documentation for the physician. Not only does this create excessive hassle for the doctor, but it also results in additional administrative processing and delays in receiving a CGM for the person with diabetes. Thus, while getting a CGM via a pharmacy benefit usually takes a matter of hours or days, it can take up to several weeks to receive one through a medical benefit.
What do states that cover CGM under Medicaid have in common?
Diabetes prevalence: While it might be expected that states with the highest diabetes prevalence would also have the greatest investment in diabetes tools, this is not the case. Among the 14 states where at least 12% of adults have diabetes, only 6 of them (AR, NM, IN, OH,TX, and WV) cover CGM under Medicaid for people with both type 1 and type 2 diabetes.
Medicaid spending: Five of the top 10 states with the highest Medicaid spending (above $15 billion in total) do not cover CGMs for both people with type 1 and people with type 2 diabetes. This approach is not cost-effective because CGMs account for only 1.1% of the total cost of diabetes, while the costs of treating complications and lost productivity -- both expenses that would be reduced with widespread CGM use -- account for 73.1% of total diabetes costs. In addition, using a CGM has been shown to be cost-effective for individuals with diabetes.
Should my state’s Medicaid program cover CGM?
We believe that all people with diabetes who receive healthcare from state Medicaid programs should have access to CGMs in order to improve daily management of diabetes, reduce healthcare spending on hospitalizations and long-term complications, and enhance quality of life. All people with diabetes, regardless of type 1 or type 2 diabetes, can benefit from using intermittent or real-time CGM.
We also believe that the eligibility requirements for obtaining CGM through Medicaid should ensure reasonable out-of-pocket costs and minimal processing delays. Medicare has recently adjusted their eligibility requirements to make CGMs more accessible but many Medicaid programs still require 3-4 blood glucose tests per day. In Alabama, Arizona, Florida, Georgia, Hawaii, Kansas, New Jersey, and DC Medicaid recipients with diabetes do not have any form of CGM coverage.
The expansion of CGM coverage in California will help many people with type 1 diabetes access these valuable devices, but there are millions of people with type 2 who can also benefit from CGMs. California and the 21 other states mentioned above must expand Medicaid coverage of CGMs to improve diabetes management for all people with diabetes. We hope to see more states advance CGM access under their Medicaid programs. diaTribe will continue to advocate for CGM access for people with diabetes.


